Introduction
For multiple myeloma patients who are eligible for transplant determined by age and physiological reserve, autologous stem cell transplant (ASCT) following induction chemotherapy is considered as frontline treatment due to the better depth of response, progression-free (PFS) and overall survival (OS). Bortezomib is effective as part of a multi-agent induction regimen prior to ASCT as supported by long-term analysis with survival benefit. However, the role of Bortezomib and Thalidomide consolidation remains controversial. In New Zealand, Bortezomib was funded for up to nine cycles in front line setting. To maximise Bortezomib exposure, patients were typically given four to five cycles of Cyclophosphamide-Bortezomib-Dexamethasone (CyBorD) induction and later received the remaining number of cycles as consolidation after ASCT. Here we present our real-world data on patients who had CyBorD induction followed by ASCT and VTD consolidation.
Method
Data from 3 centres across New Zealand (Waitemata District Health Board, Counties Manukau District Health Board and Northland District Health Board) were extracted from the patient electronic database. All patients with multiple myeloma under the age of 70 who received CyBorD induction and ASCT as frontline treatment between 1 January 2013 and 31 December 2019 were included. Treatment response was determined as per the International Myeloma Working Group criteria and survival time was determined from the time of commencement of CyBorD. All statistical analyses were performed using IBM SPSS version 20.The data cut-off date is 10th October 2019.
Result
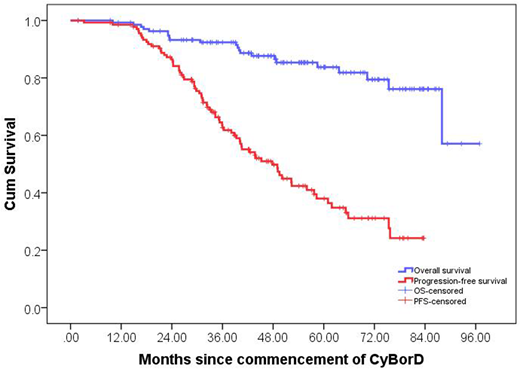
A total of 263 patients were identified from the 3 centres who were aged <70 and received frontline CyBorD. 125 patients did not proceed with frontline ASCT due to comorbidities, patients' choice, or progressive disease. In total, 138 patients received ASCT following CyBorD induction from the 3 centres. The median age was 60.8 (range: 34.2 - 69.8) and 86 (62.3%) were male. 69.6% of the patients were European, 9.4% were New Zealand Maori, 10.9% were Pacific Islanders, and 5.8% were Asians. The international staging system (ISS) was able to be determined in 89.1% of the patients, and 48.0% and 21.1% of them were ISS II and III, respectively. FISH cytogenetic results were available in 91.3% of the cases, and 13.5% of these patients were deemed to have high-risk disease (del(17p) 7.9%, t(4;14) 3.2%, t(14;16) 1.6%, and concurrent del(17p) and t(4;14) 0.8%). The median number of cycles given in induction was 5 (range: 4 - 9). 60.1% of the patients achieved at least a very good partial response after induction, and this was increased to 84.1% after ASCT and 87.7% after consolidation. Complete response was increased from 22.5% after induction to 30.4% after ASCT and 40.6% after consolidation. After a median follow-up of 54.5 months (range: 1.8 - 96.9 months), the median progression-free survival was 47.8 months and the median overall survival was not reached (Figure1). The estimated 2 and 5-year survival were 93% and 84%, respectively. Thalidomide was added to the induction regimen in 19 patients and this was commonly done due to the presence of high risk clinical features or suboptimal clinical response as determined by the treating clinicians. These patients did not appear to have an inferior treatment outcome with a comparable median PFS (median 42.2 vs 49.5 months, p = 0.291).
Conclusion
Our real-world data shows that Bortezomib-based consolidation following ASCT improves depth of response and results in favourable long-term outcomes. Patients who required the addition of Thalidomide during induction due to suboptimal response do not appear to have an inferior long-term outcome.
Jackson:Abbvie: Honoraria. Chan:AbbVie: Membership on an entity's Board of Directors or advisory committees; Roche: Other: TRAVEL, ACCOMODATIONS, EXPENSES (paid by any for-profit health care company); Amgen: Other: TRAVEL, ACCOMODATIONS, EXPENSES (paid by any for-profit health care company); Celgene: Other: TRAVEL, ACCOMODATIONS, EXPENSES (paid by any for-profit health care company); Janssen: Membership on an entity's Board of Directors or advisory committees, Other: TRAVEL, ACCOMODATIONS, EXPENSES (paid by any for-profit health care company), Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal